5 Questions With . . . Psychology’s Charles Sanislow on Psychopathology

This issue, we ask “5 Questions” of Charles “Chuck” Sanislow, assistant professor of psychology, who is both a clinical psychologist and a psychopathologist and studies a variety of mental illnesses and the approaches used to diagnose and treat these ailments.
Q: You are clinical psychologist but also a psychopathologist. Can you explain that second title for us?
A: Psychopathology is literally “the pathology of the mind.” To study disorders of the mind requires a variety approaches. Biology and brain systems tell us a lot about when things are working right in the brain, and how they go wrong. We also need cognitive theories to help us understand mental processes, such as disruptions in working memory and emotion regulation. Behavioral approaches inform how our experiences and thought processes may be conditioned and shaped by interpersonal processes.
Q: What do you hope to achieve with your research?
A: Much of my work has aimed to improve clinical diagnosis. Most psychological disorders as we now know them are based on symptoms and behaviors that seem to cluster together forming a “syndrome.” The causes and mechanisms of these patterns are not well known. One artifact of the current approach to clinical diagnosis is that patients often meet criteria for several mental disorders at once. What does it really mean to say that a person has two different kinds of depression? Are these differences really qualitative? Are the mechanisms independent? These are the types of questions that we ask in my research in the Cognitive-Affective-Personality-Science (CAPS) lab.
Q: How do you approach these questions in your day-to-day research activities?
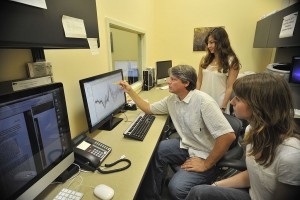
A: The majority of the research is focused on mental disorders with disturbances in mood and affect and that are moderated by stress or temperament. For example, we study depression and anxiety, including posttraumatic stress disorder and personality disorders such as borderline. We find a tremendous overlap in the features and mechanisms of these disorders. Comparing combinations of these disorders is one way to begin to clarify core processes that may cut across a range of disorders. We use advanced statistical procedures with diagnostic and functioning data from large clinical samples. We also recruit patients from the community who have experienced traumatic events or suffer from depression or anxiety and examine their performance on behavioral tasks. For example, in one task, we challenge participants to overcome emotional distraction during a cognitive task, and identify where differences occur in working memory. Thanks to funding from NIMH and support from Wesleyan, we recently acquired the ability to measure brain activity patterns using a technique called EEG. Students play key roles in all the projects in my lab, and there are a range of opportunities for their involvement. Experiences include working with patients, programming behavioral tasks, data analysis, collecting and helping to analyze EEG data.
Q: How did you become interested in these topics?
A: As an undergraduate, I had planned to become a geneticist. Because I was good with computers, I got a work-study job doing programming for outcome research at the counseling center and that was when I first learned what a clinical psychologist was. It was a fun working there, and I loved the prospect of being both a clinician and a scientist. The integration of cognitive and psychological processes with knowledge from recent advance in neuroscience make this an especially exciting time to be in the field. There is so much to learn, and the stakes are high because advances in knowledge are really important to help alleviate all sorts of human suffering.
Current diagnostic approaches serve many helpful purposes including communicating a person’s suffering in clear terms to another professional. In practice, however, clinicians often work on problems that cross multiple diagnostic boundaries, or target for treatment components common to several disorders. In clinical practice, we often look for improvement on a continuous dimension, but when we diagnose, we say someone has “it” or they don’t. More and more research suggests that psychopathological mechanisms are dimensional in nature.
My work at Yale Psychiatric Institute made clear how much we don’t know about the causes and mechanisms of psychopathology, and that there is much room to improve the diagnosis and treatment of mental disorders. When we see a person, for instance, for their first psychotic break, they may be closer to the “end-stage” of the illness. That is why some see care for the severely mentally as palliative. Knowing more about the mechanisms might help to identify how and when to intervene earlier.
Q: What is your educational and professional background?
A: I received my Ph.D. in clinical psychology from Duke University. I completed a clinical psychology internship and postdoctoral training at Yale, and stayed on as faculty member of the medical school. As a licensed psychologist, I worked mainly at the Yale Psychiatric Institute providing clinical services and serving in leadership roles to develop specialized treatment programs. With support from several grants from the National Institute of Mental Health (NIMH), my work over time became more research intensive. I’ve also worked at NIMH as Program Chief of Extramural Research in the Mood and Sleep Disorders Research. That experience really expanded my horizons to see the potential for large-scale research to make an impact on the field. But it is clear that there is still a long way to go. One reason why it was important for me to come to Wesleyan was to have the opportunity to bring students into the fray so that they could wrestle with the most pressing problems right at the start of their education.

