Future Stem Cell-based Therapies for Treating Epilepsy Explored in 3 Biology Labs
For the roughly one-third of temporal lobe epilepsy patients for whom drugs are not an option, researchers at Wesleyan are paving the way for alternative therapies using stem cells.
Faculty members Janice Naegele, Gloster Aaron and Laura Grabel, together with Xu Maisano, Ph.D. ’11, Elizabeth Litvina, B.A. ’10/M.A. ’11, and Stephanie Tagliatela, the lab manager in the Naegele lab, recently published a landmark study in the Journal of Neuroscience on the use of embryonic stem cells to treat temporal lobe epilepsy (TLE). The researchers derived neural “parent cells” in culture from mouse embryonic stem cells, and transplanted them into the brains of epileptic mice. There, the transplanted cells differentiated into mature inhibitory neurons and successfully integrated and formed connections in the host brain over the course of several months.
The paper, published Jan. 4, is available to read online.
“In these experiments, we are attempting to repair an important region called the dentate gyrus, located deep inside the temporal lobe in the hippocampus. The structures affected in temporal lobe epilepsy are important for forming memories and controlling the spread of seizures throughout the brain. When inhibitory neurons in the hippocampus are injured or die off, seizures are able to spread into other brain regions, causing more severe seizures,” explains Naegele, professor of biology, professor of neuroscience and behavior.
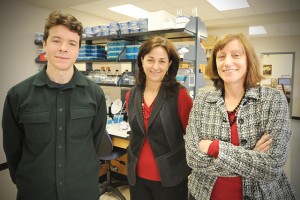
A collaboration between three different labs in the Biology Department, this study draws on the various expertise of the faculty members. Naegele is a developmental neurobiologist who is an expert on neurodegeneration and temporal lobe epilepsy; Grabel, the Lauren B. Dachs Professor of Science and Society, professor of biology, specializes in making neurons from embryonic stem cells; and Aaron, assistant professor of biology, assistant professor of neuroscience and behavior, is a neurophysiologist adept at testing the ability of stem cell-derived neurons to connect up with the host brain’s circuits and function properly.
“In all of our labs, we rely upon talented graduate students and undergraduates to do the heavy lifting and actually perform the experiments,” Grabel says. “The sum total is an effective collaboration with a proven track record, making our efforts comparable to those at major research institutions.”
Maisano, who was Naegele’s graduate student, did rotations with Aaron and Grabel in order to perform the experiments described in the paper, and is the lead author on the paper. She is currently doing post-doctoral fellowship training at the University of Connecticut Health Center in Farmington.
Epilepsy afflicts more than 60 million people worldwide, including about 3 million Americans, making it one of the most prevalent neurological disorders. Most cases of TLE are acquired after an initial episode of status epilepticus (a persistent seizure) or a severe head trauma. For example, war veterans exposed to repeated bomb blasts show a higher risk of developing post-traumatic frontal and temporal lobe epilepsy. The highest incidence of TLE occurs in children under the age of 5—commonly caused by prolonged febrile seizures, brain tumors, or spinal meningitis—and in the elderly, especially those with Alzheimer’s disease. People suffering from TLE experience cognitive problems, including memory deficits, depression and anxiety.
TLE is much more difficult to treat with drugs than are other forms of epilepsy. Approximately one-third of TLE patients are resistant to antiepileptic drugs or experience debilitating side effects from long-term treatment.
“Surgery to remove the epileptic tissue may offer an improvement over these drugs, but it is only an option for patients with focal unilateral seizures in brain regions that can be safely removed without causing severe cognitive or sensory deficits,” Naegele says. “Some of the newer proposed treatment strategies based on gene and stem cell therapy offer the potential for curing the underlying defects that cause the seizures and impair cognition, rather than merely treating the symptoms of the disease.”

Naegele, Grabel and Aaron are currently carrying out research to better understand the neurological changes caused by seizures. In their Journal of Neuroscience paper, they studied functional incorporation of inhibitory neurons derived from mouse embryonic stem cells, after transplanting the cells into mice with TLE. In current work, they are beginning to explore whether human embryonic stem cells, which have been engineered to express green fluorescent protein, can incorporate into brain circuits in mice with epilepsy and control their seizures.
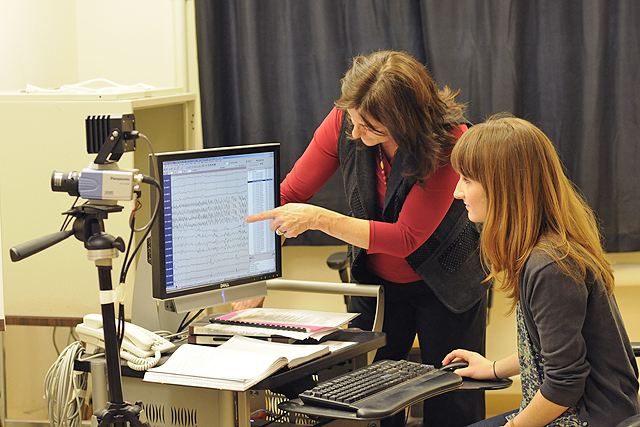
Aaron describes how the researchers take slices from the brain’s hippocampus and keep them “alive” for eight to 12 hours, bathed in a solution with tightly-controlled temperature and oxygenation.
“By viewing these slices in a microscope, we can easily see the cells that originated from the transplanted population because they express a bright fluorescent marker. Using precise manipulators, we place electrodes into individual cells, allowing us to record and control them,” he says. “These recordings allow us to characterize those neurons, and see if they are indeed similar to the types of inhibitory interneurons that are largely damaged or destroyed in epileptic brain tissue. We can also investigate whether those transplanted neurons receive and send signals with their neighboring neurons, allowing us to assess whether they have been functionally incorporated into the surrounding neuronal circuitry of the host hippocampus. Finally, by electrically stimulating these slices, we can test whether the hippocampal brain slices from mice that have received transplants are more resistant to producing epileptic-like activity compared to slices from mice without transplants.”
Translating the research being done today to actual stem cell-based therapies for TLE in humans is still many years off. Moreover, says Grabel, “The transition to clinical trial would involve extensive collaborations, perhaps with a stem cell company, and a top notch team of clinicians.”
Many questions remain, including whether spontaneous seizures can be suppressed by stem cell transplants; whether transplanted cells can differentiate into the types of inhibitory interneurons that die or becoming dysfunctional in TLE; and whether the stem cell transplants contribute to improvements in memory and alleviate anxiety symptoms.

