Johnston: What History Can Teach Us About the COVID-19 Pandemic
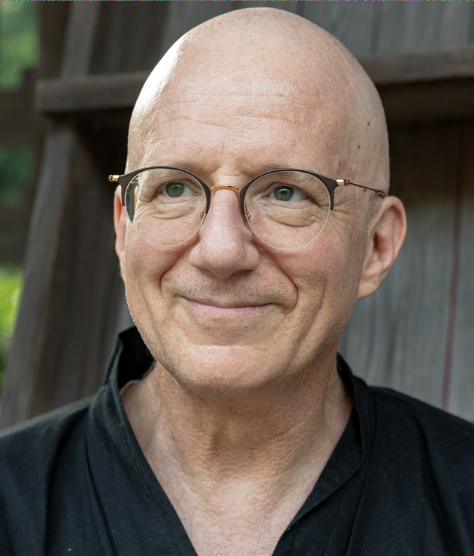
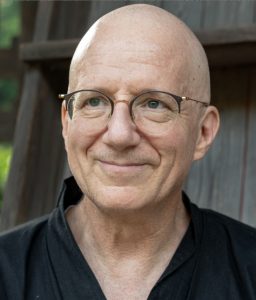
William Johnston, the John E. Andrus Professor of History, is a historian who studies disease and medicine, with expertise in epidemics of infectious diseases. In this Q&A, Johnston discusses the novel coronavirus outbreak and what can be learned from the past.
Q: How and when did you start studying the history of disease and medicine?
A: About 30 years ago, I wrote my dissertation on the subject, which became my first book, The Modern Epidemic: A History of Tuberculosis in Japan. Around that time, people were starting to consider epidemics of infectious diseases a thing of the past that were no longer of concern to us, but then HIV took off. I’ve continued to study and teach on the history of disease and pandemics ever since.
Q: Please tell us about the course you teach.
A: It’s called Critical Approaches to the History of Disease and Epidemics. Ironically, almost every year I’ve taught it, the world has seen another major epidemic. I’m offering it again this semester, and our first day of class was January 23, just as the novel coronavirus was emerging as a serious threat in China. Seeing that this was coming down the pike, I adjusted the direction of the course to incorporate a combination of historical readings and articles from contemporary medical journals. For example, I gave students one reading on the plague and how it went pandemic in the Middle Ages—what it took for that to happen.
We then studied the H1N1 outbreak in 2009, which included a piece about why the WHO was loathe to call that a pandemic. We used that as a basis from which to discuss the politics around the term “pandemic,” which the WHO refused to use until last week. I’ve assigned several articles from medical journals about COVID-19 so students can keep up with the latest science. And I’ve just assigned Pale Horse, Pale Rider, a wonderful novella published in 1939 by Katherine Anne Porter, about the experience of a couple who becomes sick during the influenza epidemic in 1918. Through these readings and discussions, I’m trying to get students to think in terms of how we can understand what’s going on around us by placing it into a historical context. To really understand epidemics, we need to have multiple epistemological perspectives in hand at the same time—including epidemiological, cultural, social, economic, and political perspectives.
Q: It seems like many government officials and others initially underestimated the seriousness of the COVID-19 outbreak. To what do you attribute the failure to learn from past epidemics?
A: In the fall of 2018, I taught a seminar on the centennial of the 1918 flu pandemic—the largest mortality event of the 20th century, by many estimates killing more people than World War II. Yet at the time, there was no talk about this important anniversary in the news. It was crickets. Unfortunately, I think public health is not a sexy topic; it doesn’t grab people’s attention. I believe that without some sort of an ideological bent, where you can point to a bad guy who’s after us—like in the war on terror—people are less likely to pay attention. We haven’t made heroes of the doctors and nurses who take care of patients at times like these, the way we publicly honor military leaders. There’s also a stigma attached to disease, where people are reluctant to speak about family members who are affected.
Q: We’ve heard this pandemic compared to the 1918 flu as the closest historical event. Do you think that’s accurate, and are we any better off today with advances in technology?
A: I do think there are many similarities to the 1918 flu. Though they’re caused by completely different organisms, the unfolding of symptoms looks very similar. Both are caused by aerial transmission—it’s floating around us; we don’t know where it is or how many are infected.
Certainly our medical technology has improved significantly since 1918. But I was talking to a doctor yesterday, who compared our hospitals to hotels. We have a for-profit system, which means maximizing occupancy at any one time is going to maximize profit. As a consequence, we don’t have a lot of leeway in our system. Over 80% of ICU beds in the country are already taken right now. We are going to have a situation where within two months, physicians are going to have to make difficult decisions about who lives and who dies. For the individuals who get the care, yes, technological improvements are going to make a huge difference. But if you don’t have access to it … it will just be too bad. It is terrible to force physicians to make such choices, but that is the system we have.
Q: You’ve also studied issues of disease and inequality. Why are economically disadvantaged people more likely to suffer during outbreaks?
A: People who are economically and socially disadvantaged are much more likely to suffer than people who are better off. We saw this in the 1918 flu and other pandemics. First of all, in today’s pandemic the costs of becoming very ill and winding up in a hospital in the US can become astronomical. Many Americans can’t afford healthcare as many have no insurance or are underinsured. Imagine the bill someone would get for three weeks in an ICU.
Economic disparities also affect people’s abilities to self-isolate. The very well-off can hop in their private jets and fly off to their private islands. Those of us in private homes can get some distance from others. But if you have seven people crowded into a two-bedroom house and one person gets sick, that’s a real problem for everyone living there. Also, the quality of nutrition can really affect people’s immune systems.
These are structural problems, and there’s not much the government can really do today that would make a difference to improve people’s living standards. There’s a notion that our health is the result of our individual choices, but that’s hardly the whole story. What’s more, we’re all in this together, and if parts of our society are suffering from bad health, that affects us all. I’m hoping that in the long run, this event might be something that can highlight how interconnected we all are.
In the short run, I think we should all be getting to know our neighbors. If you don’t know them, knock on doors up and down the street and introduce yourself. It’s important to have a network of people close by who can help out if someone gets sick. I do hope communities will rise up and help each other.

