Fins ’82 Discusses the Treatment of Brain Injury Patients and His New Book
Read more about the discussion in this Wesleyan Argus article and more about his book in this Q&A, below:

Q: What motivated you to write the book?
A: I wrote it to give voice to patients and families touched by severe brain injury and chose this genre because it was a complex interdisciplinary problem that needed a broader frame than that afforded by the typical truncated article in a medical journal. Rights Come to Mind is a story that straddles the sciences and the humanities and fundamentally is a question of how scientific advance compels us to change our views about ethics and moral obligation. I have been working with these patients and families for more than 15 years and have seen how new knowledge about the brain and consciousness made the status quo of neglect increasingly untenable and wrong. We now know that patients we thought were permanently unconscious are sometimes, in fact, conscious, albeit minimally conscious. They are often misdiagnosed and undertreated, leaving conscious individuals in the lurch. How this scientific progress informed our ethics and what it means for these patients and families is the subject of this book.
Q: How have a large number of patients with severe brain injuries been misdiagnosed?
A: That is a complex question which I explain at length in the book, but there are three key reasons for the diagnostic challenge. First, the Minimally Conscious State (MCS) is a new diagnostic category only dating back to 2002. So it’s a question about the diffusion and dissemination of new medical knowledge. Second, MCS is a diagnostic challenge because these patients are conscious but only intermittently and episodically demonstrate behaviors that show they are aware of self, others and the environment. They might track someone when they come into a room, but not do it consistently. They might respond to their name, but not when asked a second time. When families report these behaviors to the patient’s doctor or nurse, and the behavior is not repeated, what the family has “seen” is chalked up to denial or wishful thinking, when it fact the lack of a reliable repertoire of behaviors is part and parcel of the biology of MCS. The third reason for the misdiagnosis challenge is socially constructed. This refers to a pervasive nihilism towards severe brain injury which dates back to the origins of the right to die in America. Think of Quinlan, Cruzan and Schiavo, and you will appreciate that the right to die was established and sustained in the context of severe brain injury and the futility of the permanent vegetative state. The challenge is that this nihilism got over-generalized to patients with severe brain injury who were not vegetative but conscious and in MCS, a category which is often mistakenly confused and conflated with the vegetative state. Indeed, until it was its own diagnostic category, MCS patients had nowhere to go diagnostically and were de facto nestled within that larger set of patients thought to be vegetative.
Q: What research did you draw upon for your writing? Why are first person accounts so important in understanding brain injury?
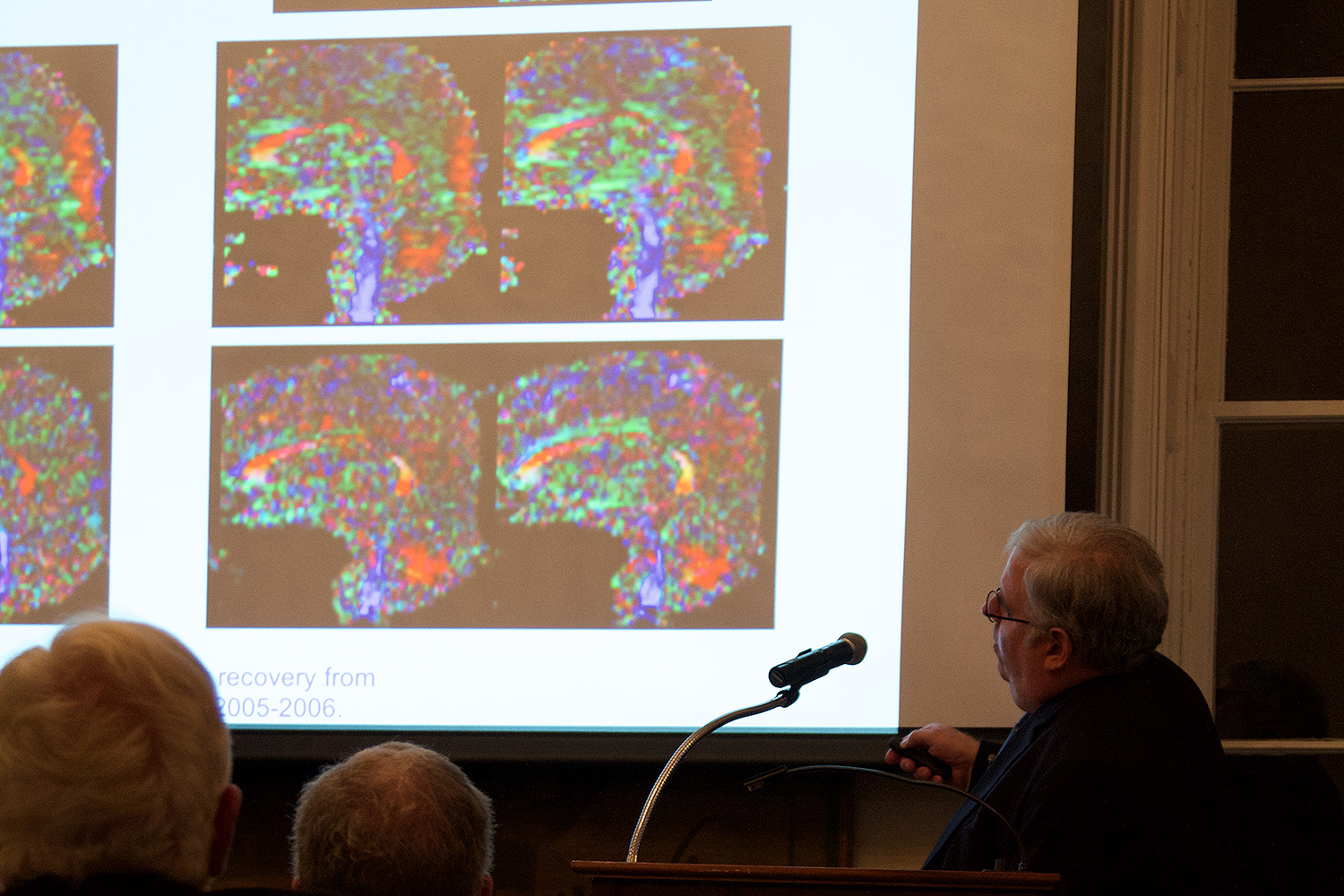
A: Three basic sources. First, from my role as a physician-investigator and co-investigator on a number of clinical trials including the first use of deep brain stimulation in MCS, which we published in Nature. I have also been a co-author of neuroimaging studies on patients with severe brain injury and co-direct C.A.S.B.I., the Consortium for the Advanced Study of Brain Injury at Weill Cornell and Rockefeller. This has given me an insider’s perch on the neuroscience of disorders of consciousness, something which is really a Cornell Medical school area of inquiry dating back to the work of my teacher Dr. Fred Plum, who co-originated the Persistent Vegetative State in 1972 and the Locked-in-State in 1966. Fred was a professor and later a collaborator. I was very lucky to be steeped in this tradition and have this focus on the brain and mind having trained here. A second source of research was my work in medical ethics in general, and the newer field of neuroethics, which I have had a chance to shape as it has evolved. And the third source is a Wesleyan one. I have sought to bring these two threads, of neuroscience and neuroethics, together with family narratives, drawing upon my earlier training at Wesleyan in the College of Letters. As is well appreciated, C.P. Snow spoke of the two cultures, and this is a two-culture book. You can’t study this problem in a purely scientific frame; it needs the broader context of the humanities and social sciences to be fully apprehended and contemplated. I have sought to bridge these two cultures in the book in a synthetic fashion in order to explicate the complexity of the problem, be true to the science and the stories, and use this approach to engender concern and compassion for a very vulnerable and marginalized population of patients who are not served well by the healthcare system.
Q: What obstacles have arisen in furthering brain injury research?
A: As I have said, these patients suffer from a pervasive nihilism that often precludes their receipt of emerging therapies that can make a difference. We also have the challenge of doing research in patients who, by virtue of their brain state, may be unable to provide consent. This was a major focus of my scholarship, and I spent 10 years trying to untangle the conflation of informed consent with respect for personhood, in order to allow research to proceed. Clearly to do research without asking for consent, or to do so over an objection is a disrespect of personhood and morally proscribed, but it is quite another issue to require consent as a proxy of respect for persons when the subject is unable to provide it, especially when the object of the intervention is to help restore functional communication and agency, which is precisely what we did in the DBS in MCS trial. This is apparent in retrospect but was a challenge to argue prospectively, but I tried to do so and we did the trial.
Q: What communication advances have been made for those patients with severe brain injuries?
A: We have developed a range of neuroprosthetics that can help facilitate communication. Drugs, neuroimaging and deep brain stimulation are emerging interventions which may help patients overcome what has been described as cognitive motor dissociation in which the patient is unable to get what might be going on inside his or her head, out to the outside world. This is a more generic problem than brain injury alone and could also be relevant to children with autism, for example, whose verbal and even emotional output might not reflect the richness of thought within their brains. Perhaps what we learn about cognitive motor dissociation in brain injury will be relevant elsewhere. I certainly hope so. Indeed one of my goals is to break down those proverbial silos that exist even within the confines of neuroscience so that investigators in seemingly disparate sub-fields can learn from each other and collaborate productively across traditional categorizations of knowledge.
Q: What changes have you seen in the rights of those patients with brain injuries and their families?
A: To date, not too much, and Rights Come to Mind was written to assert that consciousness is a right, that is, patients who are conscious have a right that it be recognized and if it is liminal, that it be augmented so that they can be more fully engaged into civil society and into the nexus of their families and community. This integration, which is wholly consistent with the legislative intent of Americans with Disabilities Act and the ethos of UN Convention on Disability, happens through the restoration of functional communication, which in turn allows for reintegration of these people into community. We help them communicate and help restore human community, no small task, but a critically important one. This kind of argumentation has been my focus at Yale Law School where I am now the Solomon Center Distinguished Scholar in Medicine, Ethics and the Law, commuting up to New Haven to work with law students. We are writing papers to address current challenges, but I also hope I am preparing future leaders in the law for a new civil rights movement which will take the needs of these conscious individuals seriously. We have to look to the future because, like all civil rights challenges, this will take time. It is a multi-generational task both for medicine and the law, but it is really time we get the discussion started and give these people their civil rights so that they get the protection of the law, laws like the ADA and ultimately the care they need. That was what I hoped to catalyze by writing this book. Neuroscience has been a wake-up call, reminding us of our neglect of these folks amidst so much promise. We must not tarry in reintegrating them into society, segregated as they currently are in chronic care far from scientific advances and their communities.

